My Story: An Unexpected Journey Into The World Of Medicine
First and foremost, I cannot stress enough… I am NOT a doctor. I was a patient given a devastating diagnosis with what doctors explained was an equally devastating fate. After my initial pity party, I decided to bury myself in research because I simply could not believe there was nothing that could be done to make myself better. Several of my doctors became concerned with the fact that I wasn’t “accepting” my condition. After much prompting, I finally agreed to go to counseling. What I learned was that I had very much accepted my diagnosis; after all, it took over four years to get an accurate diagnosis officially confirmed. However, I had quickly rejected the status quo fate that was assumed to accompany the disease. The following is a short synopsis of my story.
 Before Mito Took Its Toll – 2010
Before Mito Took Its Toll – 2010
It Started Mild
Mere months after arriving at a new military base, I began to develop several unexplained symptoms. At first, my doctor was not concerned; a physical exam and lab work showed no sign of any potential health issue and looking at me, no one would ever guess anything was wrong. But over time, things got progressively worse. It started subtle; numbness and tingling in my extremities that started with my toes and tips of my fingers and, over time, seemed to take over more and more of my feet and hands. Since I was otherwise healthy with no risk factors, neuropathy wasn’t even a consideration. I was told that maybe I was tying my boot strings too tight. Next was the onset of spontaneous and painful muscle spasms. At first they were short-lived and easily dismissed and often prompted the consumption of a banana (assuming a potassium deficiency was likely the issue). But within months they became excruciating and debilitating distortions of my limbs, locking them into painful positions often requiring someone to help physically manipulate the limb back to position and hold it there until the spasm subsided. Then the migraines kicked in. I had juvenile migraines growing up but only had two since high school. Imagine the shock when, after over 12-years of being migraine-free, I realized a massive migraine was beginning. During these initial months, I started noticing that even a brief walk down the hall would make me breath a little heavier. Eventually this turned into not being able to run my mile-and-a-half without completely getting winded and becoming lightheaded and faint, and finally, having my lower leg muscles get tighter and more contracted with each stride until the muscle would lock up and cause me to fall due to a lack of muscular control. At this point, I had undergone significant medical work ups with no definitive answers. Most tests returned normal results. Other tests would reveal minute abnormalities but not enough to convince me of the diagnoses all of my doctors were throwing at me… along with all of the associated prescriptions meant to treat them. So as my condition continued to decline, I continued to seek referrals and more testing. I knew we didn’t have the right answers yet.
My First Crash
January 14, 2010, was the “trigger” that changed my life forever. I was called in to get the H1N1 vaccine. Being military, receiving vaccines is part of your required duties. The previous six months, I had received a vaccine in June, two more in September, and two more in October, one of which was the live, nasal administered seasonal flu vaccine. I balked a bit about it, even telling the nurse I hadn’t had the flu since I was 18 so I thought I was good. Her response, “it’s mandatory” and said I was required to report for the vaccine by the end of the day.
Less than 40-hours after administration of that vaccine, I had what Walter Reed later documented as an adverse event to the H1N1 vaccine. I had spontaneously become ill to my stomach, got dizzy and my vision went black; though I was still coherent and speaking. Still with no vision, I was trying to get to a place to sit down. My knees kept buckling and I had to be physically held up. Having never blacked out before, somehow I knew… “I’m going to black out, I’m sick, I’m going to black out!” The person assisting me grabbed me to hold me up. I remember trying with all my might and strength to regain my hold on him as he lifted me up but it seemed a useless struggle. I was not quite dead weight but quickly approaching it. For a moment, I regained standing and he says he looked me right in the eye and said, “Are you okay?” I remember telling him yes but I still had no vision. I just wanted to lay down. Thinking I was “okay,” he let go of me for a moment and I remember an immediate sensation of falling, but I don’t remember hitting the ground.
All of this occurred in less than a minute. I regained consciousness in just as quick a time. But what I woke up to was a completely different person. I had a constant, loud ringing in the ears and my extremities were cold, numb and felt like they were vibrating profusely, though upon visual observation they seemed steady. I was extremely weak and could not stand without being dizzy and feeling like I was going to black out again. I was mentally cloudy, disoriented and my brain felt slow and heavy.
I was taken to my first of many ER visits, each of which proved nearly useless. I was often accused of being dehydrated (regardless of the fact that I was an avid water drinker) and\or diagnosed as having had an anxiety or panic attack (I had never experienced anxiety or a panic attack ever before). I was also always treated the same way, a bag of fluid and a prescription for anti-anxiety medication that I refused to take. Little did I know that my outward refusal of anxiety medication had triggered my medical record to be documented as me being a “non-compliant” patient. Additionally, I was labeled with “conversion disorder,” which basically means they consider your unexplainable symptoms as psychological manifestations (a\k\a it’s all in your head). It shocked me to learn how I was being viewed by the medical staff. I also mistakenly assumed that with all the “drug-seekers” showing up with unverifiable conditions, that I, being a patient not seeking drugs, would be taken more seriously by medical professionals. What I learned later was that their skewed view of me caused them not to consider “classic symptoms of neurotoxin exposure” which would have ultimately led to an accurate diagnosis and possibly would have limited my long-term chronic exposure.
While at this first ER trip, I had a series of the involuntary muscle spasms that were witnessed by staff and doctors. One physician was intrigued by my spastic muscles, but after hours of evaluation, they couldn’t find anything wrong with me. Despite my position otherwise, my episode was documented as my first anxiety attack. Being discharged, I got up to leave and collapsed in the hall just steps from the bed. They helped me back and started a re-evaluation, to no avail. So once again I got up to leave, only to collapse yet again. Describing my intense weakness and sudden loss of vision followed by the collapse, a nurse hooked me back up to the monitor and had me get up and walk down the hall. She recorded the first sign of something actually “wrong.” Upon standing, my heart rate jumped up and continued to climb until I would eventually collapse. Despite this new finding, I retained my diagnosis of anxiety attack and was sent on my way.
Mounting Symptoms and a Growing List of Diagnoses
After several similar episodes sent me back to the ER over the next two weeks, I was eventually referred to cardiology for the heart rate issue and neurology for the involuntary muscle spasms. Following testing, I received two diagnoses in one week: Postural Orthostatic Tachycardia Syndrome (from a Tilt Table Test with no need for Nitroglycerin Challenge) with notations for Paroxysmal and Paroxysmal Atrial Tachycardia and Syncope; and Dystonia (based on observation and my videos of episodes). It also resulted in an onslaught of prescription drugs trials. (Beta- and eventually alpha- blockers, mineral corticosteroids and salt tablets; and muscle relaxers, Levodopa and a couple others I don’t even remember for the Dystonia). The prescriptions only seemed to make me worse, but when I complained the doctors always wanted to try something new. In fact, as my condition declined even more, I joked I was collecting symptoms and diagnoses like a kid would collect stamps… including the side effects of all the medications. Laughing about it was my way of coping with the ever mounting stress of trying to hide just how impaired (and scared) I was becoming.
Eventually, the joking gave way to overwhelming concern as symptoms began to escalate. I was developing issues with every body system: multiple forms of Autonomic Dysfunction, diabetes, adrenal issues, unexplained chest pain, GI disruptions (both digestive and emptying and included early satiety [no appetite]), Parkinson’s-like tremors, and spontaneous mast cell activation. I also developed severe heat and cold intolerance. This was fueled by an inability to adequately regulate body temperature. I usually ran a low body temperature and felt hypothermic in mildly cool environments. The produce department of a grocery store was awful, let alone the freezer section. I also had a diminished sweat response that made me highly susceptible to overheat in even mildly warm conditions. I constantly experienced extreme Chronic Fatigue regardless of how much rest I had, shortness of breath, exercise intolerance, near constant numbness and tingling in extremities, increasing frequency and severity of migraines and tension headaches, and even altitude intolerance at as little as 800′ above sea level. I had increasing frequency and intensity of muscle spasticity that was becoming more widespread, unexplained and severe muscle pain (Fibromyalgia), muscle weakness, and eventual muscle wasting. (I became the “I’ve fallen [sat down, laid down] and I can’t get up” lady.) I also developed foot drop, gait abnormalities, listing to the right while walking (causing a workup for TIA). I had unexplained swelling and pain in my joints and increased joint dysfunction; particularly my hands, neck, back, hips, knees, ankles and feet… I know, that’s almost all of them. I developed sleep apnea, urinary incontinence and periods of excessive urination leading to dehydration. Additionally, I experienced frequent and sometimes spontaneous vision changes, eye lid twitching and uneven pupil dilation. Further testing revealed chronic and widespread inflammation all over my body (both myositis [muscle inflammation] and neuritis [nerve inflammation].
Physically, I felt like I was falling apart. But losing cognitive ability seemed to hit me the hardest: declines in cognitive function, short and (eventually) long-term memory issues, and a loss of an ability to control emotions. Once a very patient and even tempered person, I cried often and suddenly developed a very short fuse; I was fully capable of throwing temper tantrums like a 2-year-old. I often wished I couldn’t remember who I was or how capable I once was because I felt trapped in a body that wouldn’t let me be what I knew I could be.
The “Throw Away” Symptoms
I had several other symptoms that seemed to wax and wane with no comprehensible trigger. For a good three years, doctors constantly tossed these symptoms to the side. When I was properly diagnosed, a doctor finally explained these symptoms too; and suddenly it was so obvious. For the light, sound, smell, taste and touch sensitivities, they were episodes of “Fight or Flight.” He said, “Your body is in a state of crisis… an energy crisis; when it senses that it prepares you to escape. Think of what would happen if you had a lion trying to eat you. All of your bells and whistles would go off to alert you to the danger. But in your case, the danger is actually inside your body, so you have no conscious understanding of what the danger is.”
Then there was the sudden “chemical” intolerance; and when I say “chemical,” I mean everyday things you would never think twice about. Dry eyes (wearing contacts became impossible), eczema and severely dry, cracked and raw skin from hand soap or body wash (and anything anti-bacterial), shampoo made my scalp break out in sores, toothpaste made my gums and the sides of my cheeks peel like a chemical burn, lotion cracked my skin and made it raw, makeup broke me out within 30 minutes of putting it on. Once again, the cause was a lack of energy at the cellular level. He explained, “it takes energy to maintain the cell membrane that helps to protect the cell.” Every time a cell comes in contact with a substance that is harmful, it has to work to protect itself and to heal from the effects of the exposure. If your energy level is low, the cell can’t keep up with all of the chemical bombardment that occurs all day long, every day. As the cell membrane breaks down, cell function declines and eventually dies off. For the skin, the integrity of its structure diminishes; and as the largest organ of the body, the protection it provides begins to fail. Now keep in mind that your entire GI system is made up of these same types of cells. And think of all the harsh, unnatural and harmful things we expose our GI to. For the average person, they may never realize the harm their body fights off every day. But for someone who is energy deprived, they have an intimate understanding of just how delicate the body is.
Things Get Serious
During my pursuit for why my health was suddenly failing, I saw over 40 doctors at some of the best medical facilities in the country. As months ticked by and turned into years, I continued to get worse and no one had a clue why, not even some of the best experts in the nation. I loved my job and was terrified my failing health would end my career. I exhausted myself trying to ensure my illness did not impact my job performance. I distinctly recall the day I could no longer hide my secret; it was one of the worst days of my life.
It was September 2011 and I knew from the moment I woke up that it was going to be a bad day. I struggled to get up, dressed and out the door for squadron PT (physical training). Upon the slightest exertion I became nauseas and lightheaded. Pale and weak, I was released while everyone else headed out for a run. Arriving at my office, I attempted to get out of my vehicle when the sun hit my eyes and literally knocked me back into the seat. Eventually, I stumbled into my office and began doing absolute necessities; there was no way I was making it through the day. I leaned on the wall and felt my way to the other end of the building to drop off some files, but had to stumble to a chair and sit until I was strong enough to make the journey back to my desk. As I attempted to send out some emails, I was overwhelmed with nausea and my vision begin to fade away. Knowing I was about to lose consciousness, but having no strength to do anything more, I slid from my seat to the ground to avoid hitting my head. I’m unsure how long I was laying face down in the floor, but my next recollection was hearing someone yelling my name and for someone to call 9-1-1. Each time emergency responders attempted to move me, my heart rate skyrocketed, my blood pressure plummeted and I would start to lose consciousness and have “seizure-like” activity. After consulting with my PCM, the local ER doctor and one of my specialists, the decision was made to place me on oxygen and monitor me “in-place.” I spent the next two hours laying in my office floor before I was able to be transported. My vision was dim to non-existent at the time, but I could hear I was surrounded by my office colleagues and how upset they were, some crying at times. My limbs were heavy and numb. My muscles would contract and release randomly, sometimes breaking into a full-body tremble. Breathing was painful and it took all of my energy and effort to breath deeply enough not to hyperventilate. At this point, I had received no definitive diagnosis, though I had been assured it was nothing that would kill me. On this day, that assurance brought no comfort. I seriously wondered if I’d ever see my son again.
Finally, Some Answers… The Right Answers
Two months later, after extended testing that failed to explain an extremely low oxygen diffusion rate, I posed a question to my pulmonary doctor; “If I am only diffusing 68% oxygen, why do I show 98-99% oxygen saturation when you put that little red light on my finger?” It was like a light bulb went off. His eyes got really big and he said, “I am so sorry… Sometimes it’s the little things you miss. You don’t have an oxygen diffusion issue; you have an end-process metabolic disorder!” I’m sure I had a puzzled look on my face before he clarified his epiphany, “You have plenty of oxygen, your cells just aren’t using it. So you have an excess of oxygen in your blood when it returns to your lungs and only 68% can diffuse over… It’s like a glass half full, only so much more oxygen can fit.”
With this new hypothesis, I was sent for yet another series of tests. I had already had several Cardio-Pulmonary Stress Tests. Each were abnormal and progressively getting worse, but the results had been dismissed as me merely struggling with increased deconditioning. I was told each time I needed to exercise more to build back my endurance, even though I suffered from extreme exercise intolerance and exercising more only resulted in me having muscle failure and syncope. I have to admit, I wasn’t expecting to get much out of the first appointment, but this Stress Test would be very different. I was seeing a brilliant physician at UC Davis Sports Medicine Clinic that had extensive and specific expertise in aerobic and anaerobic function. After barely being able to struggle through 8 minutes before my leg muscles seized up and I was on the verge of losing consciousness, he sat me down with an oxygen mask and said, “I know exactly what is wrong with you.” (I had heard that many times before.) “You have Mitochondrial Dysfunction.” (I had NOT heard that before.) I had received so many inaccurate or incomplete diagnoses, I did what I had learned I had to; I pulled out my list of symptoms and requested the doctor explain the condition thoroughly and describe how that particular diagnosis accounted for not just some, but each and every symptom I had acquired. He kindly and patiently began an in-depth explanation, even diagramming out more complex aspects of the interrelated disorders involving multiple systems. For the first time, every symptom was explained; none were tossed to the side as being irrelevant or chalked up as some other unrelated issue. In that moment, I was overwhelmed with a huge sense of relief. I finally knew what I was facing… now I could finally fix it. But then, he said something no patient ever wants to hear. “The condition is permanent and degenerative . I’m afraid you are only going to get worse.” My relief of finally knowing what was wrong suddenly vanished into devastation. I was 37 years old and already spending significant periods of time practically bedridden. How on earth could things get worse?
Fighting Against a Broken System
After some initial research, I was thoroughly convinced that I had a Mitochondrial disorder. However, these conditions were considered extremely rare and my core team of doctors and specialists balked at this hypothesis. In fact, they wouldn’t approve the request for a muscle biopsy to confirm the diagnosis and didn’t send me back to the UC Davis doctor for nearly a year. Thus my journey into the world-wide-web of medicine began. I spent the next year burying myself in research; everything from physiology and cellular biology to clinical research and journal articles on the latest advances in understanding Mitochondrial disorders. I was desperate for knowledge, but I had no idea how important my own research would be to my future health.
During the year following my hypothesized diagnosis, my condition was now being referred to as Generalized Autonomic Dysfunction Affecting Multiple Systems. I continued to attempt to convince my medical team my condition was Mitochondrial in nature. I was told that even if I was officially diagnosed with Mitochondrial Dysfunction, there was no cure; therefore, my treatment options would be the same regardless. Treatment consisted of “symptom management with the goal of hopefully providing improved quality of life.” So my new treatment protocol began.
I continued to undergo more extensive testing at several facilities across the nation and eventually spent three weeks at Walter Reed for a comprehensive evaluation with 14 different fields of medicine. I had multiple specialists, none of whom had any in-depth understanding of Mitochondria, and each offering one or more prescriptions to “help.” I topped out at 15 prescriptions and had doctors discussing writing prescriptions for the side effects of prescriptions. I ballooned from 145 pounds to 196 pounds, was experiencing cardiac and blood pressure issues, pulmonary issues and decreased oxygen diffusion rates, GI issues, and devastating cognitive and memory impairments. I was now pre-diabetic with a prescription of Metformin waiting in the wings and a series of other unexplained lab abnormalities that doctors couldn’t even explain. Despite their efforts, my condition continued to deteriorate but quicker than ever before. It became apparent that the experts were grasping at pharmaceutical straws and their attempts at symptom management were only making my condition worse. Being as sick as I was was not an option. Something had to change.
*This slideshow takes you from:
- Summer 2009, a happy, healthy OTS graduate
- Mar 2012, homebound and bedridden toxic mess
- Jun 2012, a constantly “crashing” patient at Walter Reed
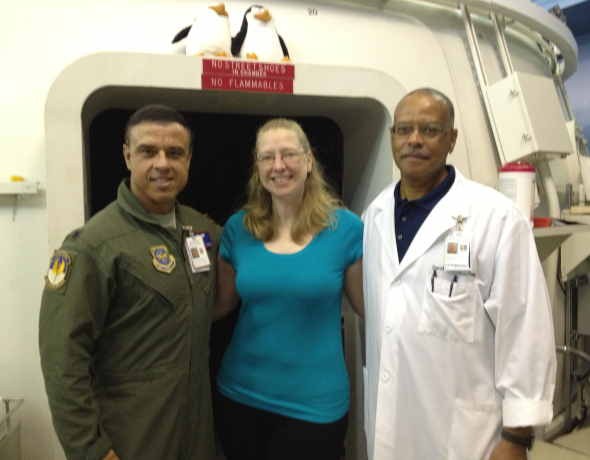
- Starting daily Hyperbaric Oxygen Treatments in conjunction with Six Pillars Protocol
- Dec 2012, still weak but back on my feet (6 months into Six Pillars Protocol)
- Apr 2013, my first ever attempt at belly dancing (10 months of Six Pillars)
- Jul 2013, already showing more strength and weight loss; completing my 136th Hyperbaric Oxygen Treatment (13 months of Six Pillars)
- Jul 2015, continuing to live my Six Pillars Protocol
- Oct 2019, Six Pillars Protocol as a way of life
*NOTE: My hair has not been colored in any way in any of the photos on this page. As my illness progressed, my hair became dark, dry and ashy in color. My face was often yellow in color with episodes of what my Team at Walter Reed referred to as “the orange mask.” My lips were often purple, a sign of hypoxia. Acne became a constant battle; a sign of toxic issues in the body.
Hope… With a Little Help From My Friends
After one of my labs came back with a note stating that the lab value was indicative of a Mitochondrial Dysfunction, I was finally sent back to the UC Davis doctor for a muscle biopsy. The results confirmed Mitochondrial Dysfunction and also uncovered evidence of a toxic exposure. Eventually, an occupational health investigation determined I had been chronically exposed to improperly used pesticide. Though accidental, I had been systematically poisoned for 3-1/2 years. The pesticide (active ingredient Fipronil) had twelve (12) known modes of action that affected Mitochondrial and/or other metabolic pathways and there was no known antidote.
I began to focus my research on what I personally could do to detoxify my system and support proper Mitochondrial function and other related body systems. After discussing it with my pulmonologist, one of my most trusted physicians, I made the decision to ween myself off all the prescriptions and seek a more natural solution. I had little support from the medical community that had previously been so eager to “help.” But I was blessed with a few exceptions, four doctors who knew I had diligently tried everything asked of me. Mitochondrial Dysfunction was far from their areas of expertise, but they had a level of medical expertise far beyond my understanding. They each took time to review my research and hypotheses and to provide me with additional direction to hone in on the information I needed to formulate my own treatment protocol. I will forever be grateful to them for their part in my recovery.
Though it was tough and progress was painfully slow, often with setbacks along the way, I was determined to do all I could do for even the smallest improvement. But eventually, my progress became nothing short of amazing. In fact, having been tracking me on my electronic medical record, my Nurse Case Manager from Walter Reed contacted me to find out what I was doing because I was getting better and everyone else they were treating was continuing to get worse. Then nearly 2-1/2 years after my official diagnosis, I finally received a referral to a Mitochondrial specialist who had nothing to contribute to my treatment plan because he said I was already functionally better than anyone his clinic was treating. When I asked if there was anything else I could add to my treatment protocol he said, “just keep doing what you’re doing.”
Why This Website is So Important to Me…. It’s Because of You
My desire in creating this forum is to share the culmination (and continuation) of years of research and personal experiences of myself and others. If all I accomplish on this journey only benefited myself; well, it would be a waste. It is valuable information that was hard to piece together from a multitude of sources; and sometimes it was even harder to understand, reading medical textbooks, journal articles and research papers and taking on-line courses so I could clarify concepts. What I have studied and ventured to learn is quite complex. But the answers are relatively simple. Notice I didn’t say it was easy, there is a difference; however, it is very doable. It just takes perseverance and diligence with a dash of stubbornness in maintaining a positive attitude that you really do have the power to make a difference. Regardless of one’s current state of health, everyone can give their body the best chance to function optimally. Because everyone deserves to be as healthy as they can possibly be… and getting to your healthy best all starts at the cellular level… it starts with your Mitochondria.
Nov 2006, Approx 3 Years Before Becoming Symptomatic
Apr 2013, Approx 10 Months into My “Six Pillars of Mito Health” Protocol
Nov 2019, Approx 7 Years of Consistently Living the “Six Pillars”
I don’t want to mislead anyone. I have NOT cured my Mitochondrial Dysfunction. However, as long as I continue to provide what I know my body needs, my condition is very well managed. And though I still have to carefully craft what I do each day, I feel healthier now than before I got sick.
Whether you are otherwise healthy and simply trying to improve from where you are today, or you are facing a permanent and/or debilitating condition, what I want you to get out of this website is HOPE. With hope, we keep trying, pushing, seeking, overcoming, and succeeding; even if in the tiniest of steps. With that hope, we can seek out those things our bodies need, to provide the best opportunity at optimal function and improved health. May you find what you need to help you achieve your health goals.
Here is to your Mito health!